Cervical cancer is one of the few cancers we can effectively prevent and cure if caught early, yet it remains a global health challenge. As we observe Cervical Cancer Awareness Month in January and look forward to World Cancer Day on February 4th, there is no better time to prioritize your reproductive health. This guide is designed to empower you with essential knowledge, breaking down complex medical terms into simple, actionable steps. From understanding the role of HPV to navigating screening options, here is everything you need to know to stay safe and informed.
What You’ll Learn (Key Takeaways)
- It’s Highly Preventable: Cervical cancer is one of the most preventable cancers thanks to the HPV vaccine and regular screening.
- HPV is the Main Culprit: Almost all cases are caused by the Human Papillomavirus (HPV).
- Silent Symptoms: Early stages often show no symptoms, making regular check-ups life-saving.
- January is Key: January is Cervical Cancer Awareness Month, a time to advocate for screening and vaccination.
- Screening Saves Lives: The Pap test and HPV test can find pre-cancerous cells before they turn into cancer.
What Is Cervical Cancer?
Cervical cancer is a type of cancer that starts in the cells of the cervix, which is the lower part of the uterus that connects to the vagina. It occurs when healthy cells in the cervix develop mutations in their DNA and grow out of control.
While many cancers remain mysterious in their origins, we know exactly what causes most cervical cancers. It usually develops slowly over time. Before cancer appears, the cells of the cervix go through changes known as dysplasia, where abnormal cells begin to appear in the cervical tissue. If not destroyed or removed, these abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and surrounding areas.
The Anatomy of the Issue
The cervix has two main parts:
- Endocervix: The opening of the cervix that leads into the uterus.
- Exocervix: The outer part of the cervix that can be seen by a doctor during a speculum exam.
The place where these two cell types meet is called the transformation zone. This is where most cervical cancers begin.

Causes and Risk Factors of Cervical Cancer
The primary cause of cervical cancer is a persistent infection with high-risk types of Human Papillomavirus (HPV). HPV is a common virus that is passed from one person to another during sex.
According to the World Health Organization (WHO), nearly 99% of cervical cancer cases are linked to infection with high-risk HPVs.

Understanding HPV
HPV is incredibly common. Most people who are sexually active will get HPV at some point in their lives. In most cases, the body’s immune system clears the virus naturally without any problems. However, in a small percentage of people, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
- Low-risk HPV: Can cause genital warts but rarely causes cancer.
- High-risk HPV: Specifically, types HPV-16 and HPV-18 are responsible for the majority of cervical cancers.
Other Risk Factors of Cervical Cancer
While HPV is the main driver, other factors can increase your risk:
- Smoking: Women who smoke are about twice as likely as non-smokers to get cervical cancer, according to the American Cancer Society. Tobacco by-products damage the DNA of cervix cells.
- Chlamydia Infection: Some studies see a higher risk of cervical cancer in women whose blood tests and cervical mucus show evidence of past or current chlamydia infection.
- Weakened Immune System: People with HIV or those taking drugs to suppress their immune system are at higher risk.
- Long-term use of oral contraceptives: Taking birth control pills for a long time (5 or more years).
- Having multiple sexual partners: This increases the likelihood of HPV exposure.
- Family History: While rare, if your mother or sister had cervical cancer, your chances of developing the disease increase by 2 to 3 times.
Symptoms and Early Warning Signs of Cervical Cancer
Early-stage cervical cancer generally produces no signs or symptoms. Signs usually appear only after the cancer has spread to nearby tissues.
This is why screening is non-negotiable. You cannot wait for symptoms to appear. When they do occur, they can include:
Common Symptoms
While these signs can sometimes be caused by other conditions, experiencing them persistently warrants an immediate check-up.
- Abnormal Vaginal Bleeding: This is the most common symptom. It includes bleeding after intercourse, bleeding between periods (spotting), or bleeding after menopause.
- Unusual Discharge: Watery, bloody vaginal discharge that may be heavy and have a foul odor.
- Pelvic Pain: Pain during intercourse or general pain in the pelvic region.
Advanced Symptoms
If the cancer spreads (metastasizes), symptoms might include:
- Difficulty urinating or blood in the urine.
- Swollen legs.
- Weight loss and fatigue.
- Back pain.

Cervical Cancer Screening: Pap Smear & Diagnosis
Screening is the process of looking for cancer before a person has any symptoms. The two main tests are the Pap smear (Pap test) and the HPV test.
Screening is the most effective way to prevent cervical cancer because it can detect pre-cancerous cell changes that can be treated before they turn into cancer.
The Pap Smear vs. HPV Test
While both tests are used for cervical cancer screening, they detect different things to help keep you safe.
| Feature | Pap Smear (Pap Test) | HPV Test |
| What it looks for | Changes in cells (precancers) on the cervix. | The virus (HPV) that causes cell changes. |
| How it’s done | Cells are scraped from the cervix during a pelvic exam. | Often done on the same sample of cells as the Pap test. |
| Goal | Find bad cells early. | Find the virus before the cells change. |
How to Prepare for Your Screening
To ensure your test results are as accurate as possible, follow these tips 24 to 48 hours before your appointment:
- Avoid intercourse.
- Do not use tampons.
- Do not douche.
- Avoid using vaginal medicines, sprays, or powders.
- Try to schedule your appointment for a time when you are not having your menstrual period.
When Should You Get Screened for Cervical Cancer?
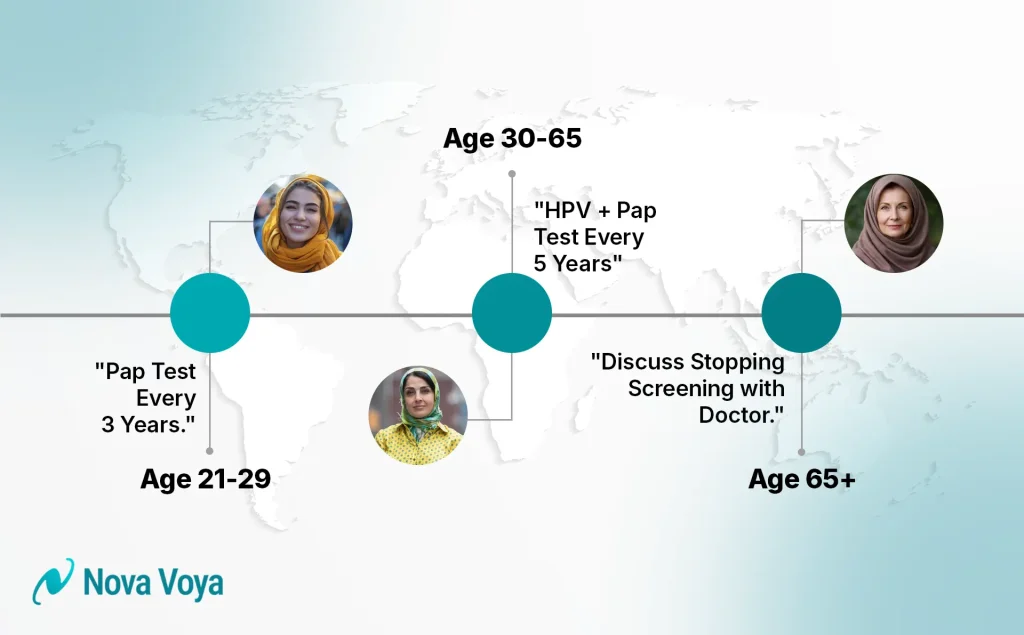
Based on guidelines from the American Cancer Society:
- Ages 21–29: Pap test every 3 years. HPV testing alone is usually not recommended for this age group unless the Pap result is abnormal.
- Ages 30–65: The preferred method is a co-test (Pap + HPV test) every 5 years. Alternatively, an HPV test alone every 5 years or a Pap test alone every 3 years.
- Over 65: If you have had regular screenings with normal results, you may be able to stop screening.
Diagnosis: What Happens if Results are Abnormal?
If your screening shows abnormal cells, your doctor will perform a Colposcopy.
- The Procedure: The doctor uses a special magnifying instrument (colposcope) to examine your cervix closely.
- Biopsy: If suspicious areas are seen, a small sample of tissue is removed. Common types include:
- Punch Biopsy: A small pinch of tissue is removed using a specific tool.
- Endocervical Curettage (ECC): A narrow instrument scrapes the lining of the endocervical canal (the area the colposcope can’t see).
Cervical Cancer Stages (FIGO System)
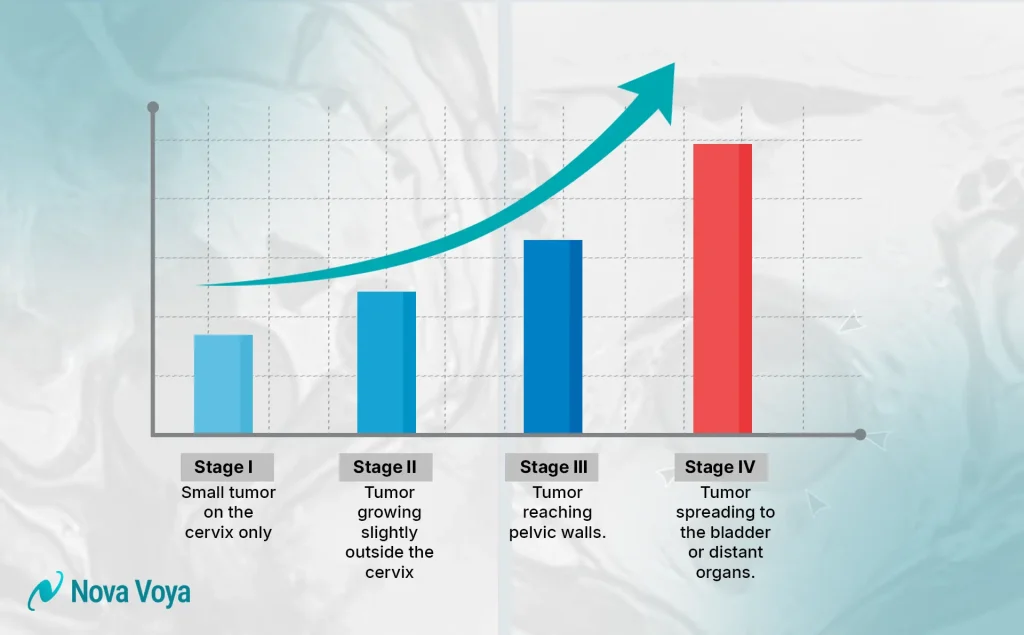
Staging is a way of describing where the cancer is located, if or where it has spread, and whether it is affecting other parts of the body. Doctors use the FIGO staging system.
Knowing the stage helps the medical team decide on the best treatment plan.
- Stage I: The cancer is confined to the cervix. It has not spread to lymph nodes or distant sites.
- Stage II: The cancer has spread beyond the cervix and uterus but has not reached the walls of the pelvis or the lower part of the vagina.
- Stage III: The cancer has spread to the lower part of the vagina or the walls of the pelvis. It may block the ureters (tubes carrying urine from the kidneys).
- Stage IV: The advanced stage. The cancer has spread to nearby organs like the bladder or rectum, or to distant parts of the body like the lungs, liver, or bones.
Cervical Cancer Treatment Options
Treatment depends on the stage of the cancer, the patient’s age, and their desire to have children in the future. The main treatments are surgery, radiation therapy, and chemotherapy.
Usually, a team of doctors (a gynecologic oncologist, radiation oncologist, and medical oncologist) will work together.
1. Surgery
Surgery is often used to remove the cancer, especially in early stages, and the extent of the operation depends on how far the disease has spread.
- Cone Biopsy (Conization): Removes a cone-shaped piece of tissue from the cervix. This can treat very early-stage cancer and allow women to keep their fertility.
- Trachelectomy: Removes the cervix and some surrounding tissue but leaves the uterus intact.
- Hysterectomy: Removal of the uterus and cervix. This is often the standard for early-stage cancer if fertility is not a concern.
- Simple Hysterectomy: Removes uterus and cervix.
- Radical Hysterectomy: Removes uterus, cervix, part of the vagina, and surrounding tissues.
2. Radiation Therapy
Uses high-energy X-rays to kill cancer cells. It can be given externally (machine outside the body) or internally (placing radioactive material inside the cervix, known as Brachytherapy).
3. Chemotherapy
Uses powerful medicines to kill cancer cells. It is often used in combination with radiation (chemoradiation) for locally advanced cancer or by itself for advanced stages.
4. Targeted Therapy & Immunotherapy
These advanced treatments work by attacking specific cancer cells or boosting your immune system to fight the disease.
- Targeted Therapy: Drugs like Bevacizumab (Avastin) block the growth of new blood vessels that cancer needs to grow.
- Immunotherapy: Helps your own immune system recognize and attack cancer cells.
Managing Side Effects of the Cervical Cancer Treatments
It is important to discuss potential side effects with your doctor before treatment begins.
- Surgery: May cause pain, bleeding, or difficulty urinating temporarily.
- Radiation/Chemo: Can lead to fatigue, nausea, skin changes, and in some cases, premature menopause or infertility.
- Sexual Health: Treatments can affect vaginal health. Your doctor can recommend therapies to help manage these changes.
Preventing Cervical Cancer
The most powerful tool we have against cervical cancer is the HPV vaccine (such as Gardasil 9). It prevents infection from the high-risk HPV types that cause most cancers.
Who Should Get Vaccinated?
- Children: The CDC recommends vaccination for preteens aged 11 to 12 years, but it can be given starting at age 9.
- Teens and Young Adults: Everyone through age 26 years should be vaccinated if they were not fully vaccinated earlier.
- Adults 27–45: Some adults in this age range may decide to get the HPV vaccine after speaking with their doctor, though it provides less benefit, as most adults have already been exposed to HPV.
Checklist for Prevention
- Get the HPV vaccine.
- Don’t smoke.
- Use condoms during sex (reduces but does not fully eliminate risk).
- Stick to your screening schedule (Pap/HPV tests).

January Is Cervical Cancer Awareness Month
Every January, the world comes together to raise awareness about cervical cancer, promote the importance of screening, and advocate for the elimination of this disease.
It is a month dedicated to education. Public health organizations, hospitals, and survivors share stories and facts to encourage women to prioritize their cervical health.
Why January Matters
Despite being preventable, thousands of women still die from this disease annually. January serves as a global reset button. It’s the time when health organizations push the message: “Get Screened.”
The Teal Ribbon
The symbol for cervical cancer awareness is the Teal and White ribbon. During January, you might see people wearing teal to show support for survivors and honor those lost to the disease.
The Global Mission: Eliminating Cervical Cancer by 2030
The WHO has launched a global strategy to eliminate cervical cancer as a public health problem. The goal is known as 90-70-90 to be reached by 2030:
- 90% of girls fully vaccinated with the HPV vaccine by age 15.
- 70% of women screened with a high-performance test by 35 and again by 45.
- 90% of women identified with cervical disease receive treatment.
Summary
Cervical cancer is a serious but highly treatable and preventable condition. It almost always stems from HPV infection, which makes vaccination and regular screening your best lines of defense. Unlike many other cancers, we have the tools to stop cervical cancer before it even starts.
If you are over 21, ensure your Pap smears are up to date. If you have children, talk to their pediatrician about the HPV vaccine. Don’t wait for symptoms like bleeding or pain; early detection via screening is the key to survival.
Take Action Today: Prioritize Your Health
Your health is your most valuable asset. Don’t let fear, cost, or a busy schedule keep you from your check-up.
- Check your calendar: When was your last Pap smear?
- Call your doctor: If it’s been more than 3 years, make an appointment today.
- Spread the word: Share this article with the women in your life—mothers, sisters, and friends.
Find Affordable Care with Nova Voya
Worried about the cost or finding the right clinic? Nova Voya is an online platform that partners with top-rated clinics and hospitals to make healthcare accessible.
- Exclusive Offers: You can find discounted checkup packages specifically in the Deals section of the Nova Voya site.
- Easy Booking: Browse and book your screening appointment directly through the platform.
What are your thoughts on the new screening guidelines? Have you had your screening this year? Let us know in the comments below!
Frequently Asked Questions (FAQs)
Yes. When caught early, cervical cancer is highly curable. The 5-year survival rate for early-stage invasive cervical cancer is 92%.
Rarely. Unlike breast or ovarian cancer, cervical cancer is primarily caused by an infection (HPV), not inherited gene mutations. However, a family history can slightly increase risk.
It is extremely rare. Since HPV is transmitted via sexual contact, those who have never had any sexual contact have a very low risk.
It can be slightly uncomfortable or cause a pinch, but it typically does not cause pain. The procedure is very quick.
No. The vaccine prevents new infections but does not treat existing HPV infections or cervical cell changes.